Precision or personalised medicine encompasses and draws on many different complex technologies. From analysis and diagnosis to treatment, prevention and even prediction, a number of fields combine in this exciting emerging field.
Biomarkers, personalised medicine and companion diagnostics
A biomarker is a measurable indicator of a biological state or condition. Traditionally, the identification of biomarkers has been an observational side product of clinical practice. However, the last few decades have seen us move into an industrialised process of biomarker discovery, capitalising on advances in areas including genomics, proteomics, and other ‘omics’ technologies, whilst aided by improvements in data analysis and bioinformatics. These advances have resulted in an explosion in the biomarker field, with new biomarkers and new classes of biomarkers, contributing to new and more precise diagnoses of diseases and conditions. These new biomarkers will improve our understanding of complex disorders such as cancers and immune diseases, as well as helping us to predict and monitor their progression, or provide insights into drug safety. Ultimately, these new approaches may allow us to detect diseases before they are symptomatic, or at a stage when they are more amenable to treatment.
A key use for biomarkers is in identifying those patients that will benefit most from a particular treatment. By matchmaking patients with the treatment that is right for them in this way, this new doctrine of personalised medicine has the potential to improve patient outcomes and experience by maximising treatment responses or by minimising adverse side effects. A key element of personalised medicine is the development of companion diagnostics (CDx). These are used to determine whether a patient is likely to benefit from a particular therapeutic agent.
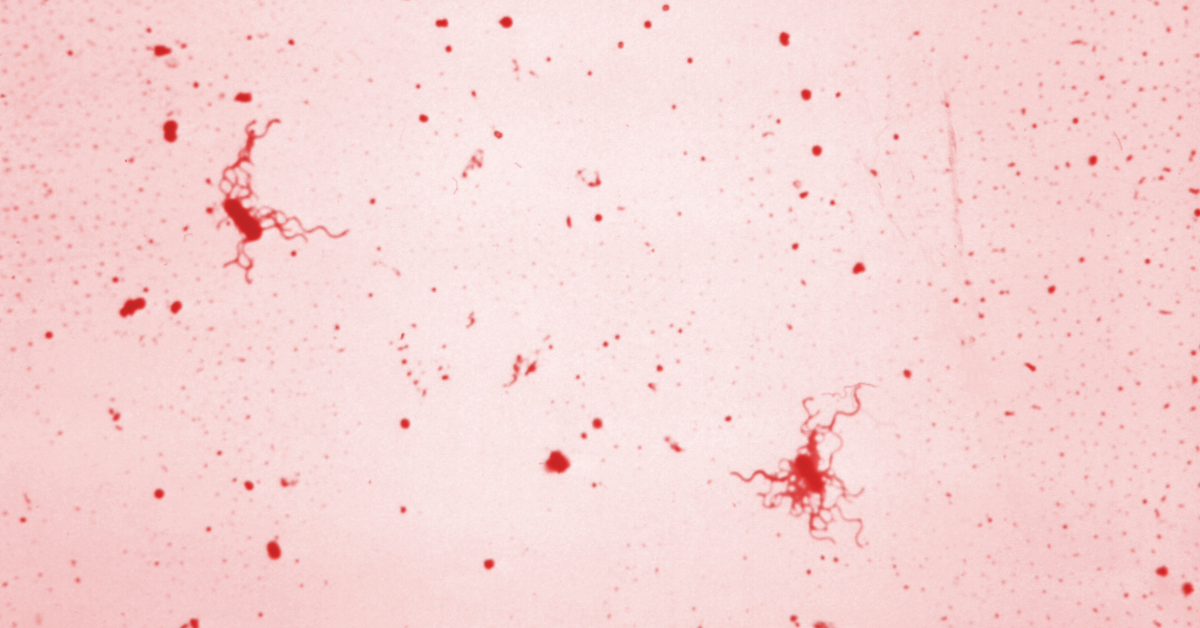
Liquid biopsy
Liquid biopsy has emerged as a powerful diagnostic tool in recent years. The term liquid biopsy refers to the use of different body fluids such as blood, urine and saliva for analysis of the health of patient, with blood samples being most commonly used. In recent years, components of blood including cell free DNA (such as circulating tumor DNA and circulating fetal DNA), microRNAs, extracellular vesicles, tumor educated platelets, and even circulating tumor cells, are increasingly being appreciated for their use in advance diagnostics, whilst benefiting from the minimally-invasive nature of this technique.
Bioinformatics, biological applications of big data
Precision medicine has been made possible by significant advances in our ability to detect and quantify changes in biology, such as small changes in the number of copies of a particular nucleic acid sequence, or the presence of particular point mutations. These advances are only part of the story, however, as their true potential can only be reached with accompanying (and sometimes guiding) advances in informatics.
Bioinformatics is a term which is used as an umbrella to encompass work that may also be referred to as computational biology or medical informatics. It is an interdisciplinary field of science that combines biology, computer science, mathematics, statistics and engineering and heralds a new approach to biomedical/biological sciences, with large amounts of data at its core.
Although many companies understand the value of bioinformatics and are investing heavily in this space, many have been reluctant to seek patent protection for their inventions. There seems to be a common misconception that software isn’t patentable. Whilst this isn’t true, the complexity of these technologies requires technical and legal expertise in both life sciences and computer sciences.
Next generation sequencing
One of the most significant technological advances in life sciences has come in the form of “next generation sequencing” (NGS). These technologies resulted in a step change in our ability to obtain genetic information. Whereas in the 80’s-90’s Sanger sequencing allowed the sequencing of a single short fragment of nucleic acid at a time (up to a few hundred bases), today’s high-throughput sequencing technologies allow the sequencing of an entire genome in a few hours and for an ever decreasing cost.
Today’s high-throughput and high-content assays enable the rapid collection of data from a large number of samples and in fine detail, transforming the nature and sheer amount of genetic data available to researchers. Technologies such as Illumina sequencing, nanopore sequencing and microfluidics are changing our understanding of the molecular basis and hallmarks of disease and fuelling the development of new diagnostics and treatments. More recently, transformational technologies such as single molecule real time sequencing and single cell sequencing are allowing researchers to cell-population summary measures and look at variability and heterogeneity in populations of cells. This has resulted in invaluable insights into the aetiology of diseases such as cancer and will transform the way medicine is practiced in the clinic.
Gene editing technologies
Gene editing technologies, such as CRISPR and TALENs have the potential to transform medicine, not only enabling us to treat diseases but also prevent them. Whilst research into editing genes has been going on for many years, new advanced techniques have made it much simpler and faster to modify multiple DNA sequences simultaneously and with high precision. Nucleic acid sequences within the body that contribute to disease can be targeted specifically and accurately, to repair or replace problems in the code, treating the patient at the genetic level.
CAR-T and adoptive cell therapies
These game-changing cancer treatments are an example of truly personalised medicine. Immune cells (particularly T cells) are removed from the patient, modified in the laboratory and returned to the patient. The cells can be modified to express a chimeric antigen receptor (a CAR), a synthetic receptor that recognises a target antigen that is found on the patient’s cancer cells.
Biological applications of artificial intelligence and machine learning, such as image processing (e.g. for diagnostics)
Exciting developments are arising from the use of advanced algorithms and computing in healthcare. Artificial intelligence (AI) techniques such as neural networks, decision trees and deep learning are being used in a wide range of biological applications. In diagnosis, for example, AI has been used to identify disease in biopsy images, x-rays or other images, performing as well as (and sometimes better than) specialist doctors. Deep learning techniques are being used to process vast amounts of genomic and physiologic data to identify new correlations that offer new diagnostics, as well as to design new therapeutic tools. These are just a few of the ways in which AI is changing modern medicine.